
NHA to leverage CoWIN for universal immunization program: R.S. Sharma
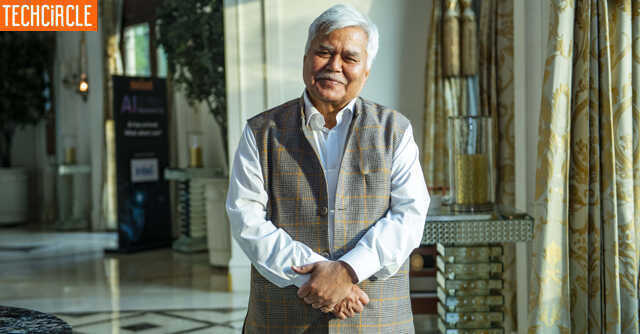

The National Health Authority (NHA) is now planning to leverage the CoWIN platform for universal immunisation program for vaccinating children and pregnant mothers against preventable diseases, said Dr R.S. Sharma, CEO, NHA in an interview with Mint. Given that only 10,000 private hospitals are a part of Ayushman Bharat PM-JAY, the government’s focus is to increase their participation under the Centre’s flagship health scheme, Sharma said. He added that with AB PM-JAY adopting a zero-tolerance approach towards fraud and abuse, 210 hospitals have been de-empanelled which were engaged in unethical practices including denial of treatment to the scheme beneficiaries, while approximately 50,000 suspect transactions were cancelled. Edited excerpts:
CoWIN platform has been able to grow alongside with the increasing pace of vaccination? May I know what other provisions are being made in CoWIN with regards to the vaccination of children and adolescents.?
With a phased rollout of the vaccination program, the CoWIN platform has adapted for quick scale in an agile manner. This is evident from the platform’s multi-fold scale up from 20-30 lakh vaccination daily during Phase 1 and 2 to a global high of 2.5 crore vaccinations in a day during Phase 3. There were multiple private and government applications (Umang, Arogya setu) which have integrated with API’s of CoWIN and provided vaccination registration service.

From January 2022 onwards, the policy for vaccination administration enabled the inclusion of adolescent population. Initially, it was for the age groups 15-17 years, followed by age groups of 12-14 years. We have already included school IDs as photo ID proofs for when the beneficiary doesn’t have any other ID proofs. For 12-17 years of age group - Covaxin, Corbevax and Covovax vaccination has been approved for children and digitally enabled for seamless registrations and recording through CoWIN. Additionally, on one mobile number, six members could be registered, allowing parents to add their children to their registered CoWIN account.
Furthermore, discussions are going on to repurpose CoWIN platform to accommodate the Universal Immunization Program for providing vaccination to children and pregnant mothers against preventable diseases.
CoWIN has emerged as a digital good with many countries willing to borrow the technology. How many countries have shown interest in learning about this technology and is NHA taking this initiative forward?

Given the importance of vaccination, India decided to adopt a completely digital approach while planning its vaccination strategy. This helped people in proving that they have been vaccinated, easing the renewal of socio-economic activities in a phased manner. A safe, secure and trustworthy proof helped people to establish when, where and by whom they have been vaccinated. Digital approach also helped in tracking the usage of vaccination and minimising the wastage. The Government of India is providing the CoWIN platform free of cost to nations interested in adopting and customising it to orchestrate vaccination in their respective nations. Over 140 countries attended the CoWIN Global Conclave to learn about this technology. Subsequent to the conclave, nearly a dozen countries expressed interest in exchanging learnings and best practices on digital administration of Covid-19 vaccination program. Zambia, Nepal, Guyana and Ethiopia are also in conversation for adopting the CoWIN platform.
As the next steps, NHA is taking this initiative forward in collaboration with the Ministry of External Affairs, by providing detailed documentation on CoWIN, and conducting functional and technical meetings with officials and experts from nations interested.
With regards to expanding the benefits AB PM-JAY to other sections of society. What is being done on these lines? What are your plans?

PM-JAY is catering to a population of 10.74 crore families included in Socio Economic Caste Census (SECC) 2011. The scheme has been implemented in 33 states and Union Territories. States/UTs in alliance with State Health Insurance Schemes have further extended the beneficiary base to 14.5 crore families (72–74 crore individuals).
Since 2021, we are using the AB PM-JAY platform to extend healthcare benefits to other categories of beneficiaries. The Employees’ State Insurance Scheme is now operational through AB PM-JAY platform (IT system, hospital network) in 157 districts. Benefits under AB PM-JAY have also been extended to Building and Construction Workers (BoCW) in 4 states – Bihar, Chandigarh, Nagaland and Uttar Pradesh. We are in discussions with nodal ministries for covering vulnerable sections like manual scavengers and transgenders.
Lastly, I would like to add that financial distress due to hospitalisation is not restricted to poor families alone. Any family not covered under a health insurance scheme will have to confront catastrophic health expenses. Many such “non-poor” families cannot unfortunately afford the premiums chargeable for commercial health insurance policies. This section of society is referred to as ‘Missing Middle’ and comprises — informal sector workers, self-employed, small business owners etc. NHA is exploring options to extend healthcare protection to the “Missing Middle”. A pilot project is being launched wherein insurance providers can use AB PM-JAY platform to cover different population groups. NHA is creating an enabling environment for beneficiary groups and insurance providers to sustainably participate in this initiative.

Since the launch of the scheme, how many private sector hospitals have come on board with NHA? What actions are being taken to bring in more corporate hospitals under the scheme?
Around 25,000 hospitals have been empanelled under AB PM-JAY, out of which 10,000 are private hospitals. They account for 55% of total hospital admissions under the scheme. However, their participation can be further improved; towards this end, NHA is adopting the following measures.
Rationalisation and liberalisation of HBP framework: NHA has recently notified the Health Benefit Packages (HBP) 2022. Under HBP 2022, we have increased the rates of more than 800 packages and introduced differential pricing to account for regional variations. Lastly, SHAs have been provided flexibility to tailor package rates depending on local context i.e., disease burden, provider availability etc.

We set up a dedicated “Hospital Operations” unit to address this problem. The HO undertook several engagement activities including field visits, webinars including co-ordinations between state and district units. This has resulted in the activation of more than 3,000 hospitals.
At NHA, we are working closely with SHAs to ensure the timely processing of hospital claims. Further, we have also launched the Green Channel Concept for payments to ensure faster disbursal of treatment-related funds to empanelled hospitals with robust utilisation and sound credentials.
Recently, our Health Minister has taken a meeting with the top corporate hospitals representative to emphasize them in adopting AB PM-JAY platform.

How many hospitals have been de-empanelled?
Under AB PM-JAY, we have adopted a zero-tolerance approach toward fraud and abuse. We have issued more than 20 advisories to the SHAs with clear cut actions outlined against fraudulent practices. Accordingly, as per information available with us, since the inception of the scheme around 210 hospitals have been de-empanelled, which were engaged in unethical practices including denial of treatment to the scheme beneficiaries.
How many fraudulent cases have you identified so far?
Approximately 50,000 suspect transactions were cancelled. This represents less than 0.2% of total hospital admissions under AB PM-JAY. It can be thus seen that the highly effective anti-fraud mechanisms are acting as deterrents for unscrupulous elements.
